
Services
After a complete evaluation of your lower extremity veins, which includes an ultrasound examination of the veins by experienced Ultrasound Technicians (RVT), our vein specialists will determine the optimal treatment for your needs. The screening takes between 5-10 minutes and checks for both deep and superficial veins for disease or malfunction.
Arterial screening helps detect blood vessel blockages or plaque buildup that puts a person at risk for ischemia in their legs, this leads to damage and can cause gangrene. Other items evaluated are aneurysms and other vascular diseases that could lead to amputation and limb loss.
Screening provides a good snapshot of what is going on in the blood vessels.

Arterial Occlusion (PAD) Treatment
Most amputations in the United States are preventable if early diagnosis and treatments were offered. We bring state-of-art technologies to cure some of the significant blockages. The usual treatments for vascular disease include balloon angioplasty (using an inflatable balloon to open the narrowed vessels), atherectomy (directional and rotational), which involves cleaning the arteries by reducing and eliminating the blockages by plaque removal and if needed sometimes stenting. Some of the blockages are long and complicated with extensive involvement where traditional approaches may fail to cure them. In such clinical scenarios we do trans-pedal revascularization (access via a foot vessel) this is done to save the legs. Advanced technologies are utilized such as IVUS (Intra-vascular ultrasound) to accurately evaluate the stenosis in difficult cases. All treatments are done in our vascular facility and under conscious sedation and local anesthetics using the insertion of the sheath via the groin.
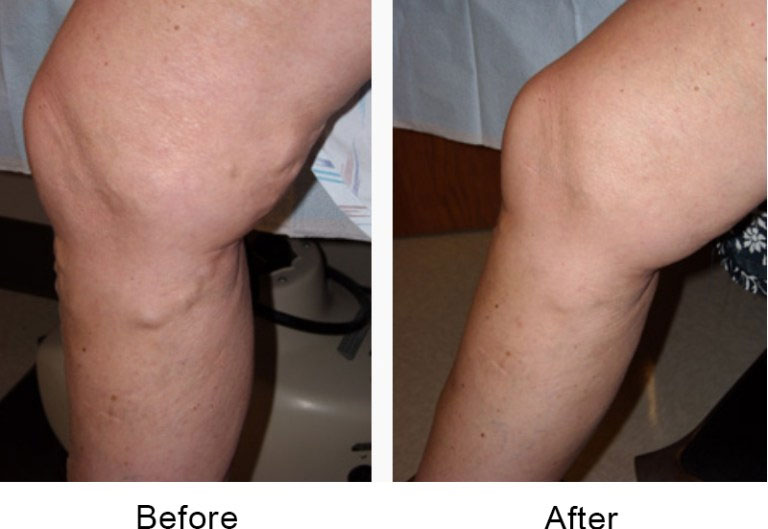
Endovenous ablation is an image-guided, minimally invasive treatment that uses radiofrequency or laser energy to cauterize (burn) and close the abnormal veins that lead to varicose veins. This state-of-the-art treatment option replaces traditional vein stripping surgery.
The procedure is performed on an outpatient basis. Using ultrasound guidance, Dr. Reddy will position the Closure catheter into the diseased vein through a small opening in the skin. The slender catheter delivers radiofrequency energy to the catheter, which heats the vein wall. As the vein wall is heated and the catheter is withdrawn, the collagen in the wall shrinks, and the vein closes. Once the diseased vein is closed, blood is re-routed to other healthy veins.
Following the procedure, a simple bandage is placed over the insertion site, and additional compression may be provided to aid healing.
Will It Hurt?
You may feel slight pressure when the catheter is inserted, but no serious discomfort. Injection of a local The actual hectic around the vein is the most uncomfortable part of the procedure because it usually requires multiple injections along the vein. The actual closure of the vein with heat is usually not painful.
Recovery
We recommend that you refrain from driving at least 48 hours after your procedure.
You may be encouraged to refrain from strenuous activities for a while. Most patients resume normal activities within 24 hours.






Acute DVT can often be treated with anticoagulation alone. However, in select cases, removal of the offending clot can help improve symptoms and prevent the development of post-thrombotic syndrome, which includes pain, swelling, skin changes, and venous ulcers.
An ultrasound is used to access the target vein, then a small catheter is used to access across the clot and a clot suctioning angiojet is used to extract some of the clots. This is normally an outpatient procedure. You will be provided with mild sedation and the area will be numb.
Recovery
Blood thinners and compression stockings are often used to encourage blood flow and prevent recurrent clotting
You may be encouraged to refrain from strenuous activities for a while
The primary goal in treating deep vein thrombosis (DVT) is to prevent the blood clot from getting bigger and preventing it from breaking loose causing a pulmonary embolism
Treatment Options Include:
Blood Thinners. This is the most common treatment. These drugs may either be injected or taken as pills as determined by your doctor.
Clot Busters. If your DVT is more serious, or other medications are not working, a clot-buster or thrombolytics may be prescribed. Administered by IV or through a catheter directly into the clot.
Filters. If you cannot take medicine to thin your blood, you may have a filter inserted into a large vein. This will prevent a clot that breaks loose from lodging in your lungs.
Compression Stockings. These help keep the swelling down. The pressure of the compression helps reduce the chances your blood will pool and clot.
Results

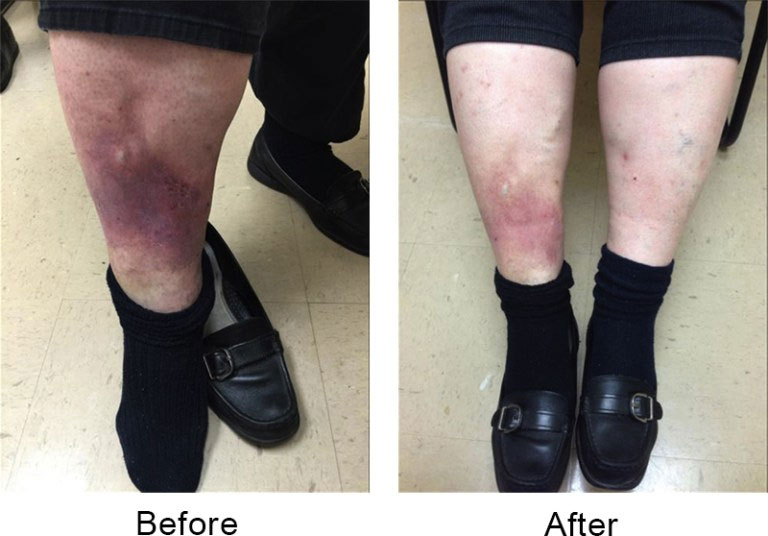
In the United States, up to 1.8 million people are afflicted with venous ulcers, which are the most common chronic wounds treated in wound care centers. More than half of the venous ulcers treated are recurring ulcerations or wounds that might have healed before but later return.
Conventional treatments for venous ulcer patients include the use of antibiotics, salves, and compression therapy. However, these treatments have high failure and recurrence rates.
Attempts to heal the skin without correcting the underlying venous insufficiency can lead to a delayed ulcer healing and recurrence.
Ocala Vein can offer you a minimally-invasive option to traditional surgery for the venous ulcers on your legs. It is the only endovenous, ablation device specifically cleared by the FDA for the treatment of incompetent perforating veins, the most common origin of your leg ulcers. This outpatient treatment can be either the primary procedure or it can be performed in addition to other outpatient leg vein procedures.


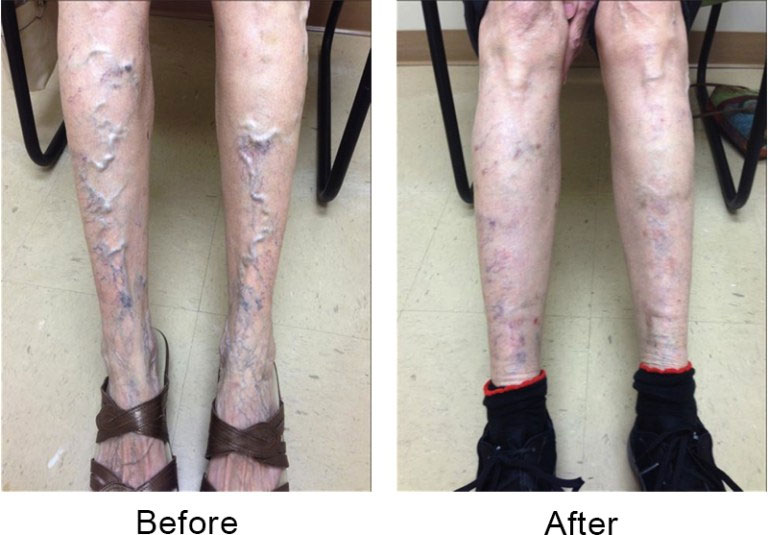
Sclerotherapy
With sclerotherapy, we inject a special solution directly into the tiny vein using a fine needle. The solution shrinks the veins and causes the blood to be redirected to other veins. The sealed-off veins are eventually absorbed by the body. Depending on the individual, we may also use ultrasound-guided sclerotherapy.
Though patients may require several treatments, sessions are quick and the patient can return to his or her normal activities immediately afterward.


What is a Cardiac Catheterization?
Cardiac catheterization (also called cardiac cath or coronary angiogram) is an invasive imaging procedure that allows your doctor to evaluate your heart function. Cardiac catheterization is used to:
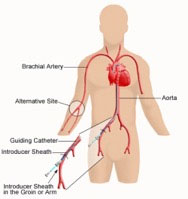
During cardiac catheterization, a long, narrow tube called a catheter is inserted through a plastic introducer sheath (a short, hollow tube that is inserted into a blood vessel in your leg or arm). The catheter is guided through the blood vessel to the coronary arteries with the aid of a particular x-ray machine. Contrast material is injected through the catheter, and x-ray movies are created as the contrast material moves through the heart’s chambers, valves, and major vessels. This part of the procedure is called a coronary angiogram (or coronary angiography). Coronary artery disease is the narrowing or blockage of the coronary (heart) arteries. After an interventional procedure, the coronary artery is opened, increasing blood flow to the heart.

Reminders about your Cardiac Cath
Will I be awake during the procedure?
Yes. You will be given a mild sedative to relax you, but you will be awake and conscious during the entire procedure. The doctor will use a local anesthetic to numb the catheter insertion site.
Cardiac catheterization is not considered a surgical procedure because there is no large incision used to open the chest, and the recovery time is much shorter than that of surgery. In some cases, surgery may be recommended afterward, depending on the results of the procedure.
Where is the catheterization performed, and who performs it?
Cardiac catheterizations are performed in the Cardiac Catheterization Laboratory. Catheterizations are performed by a specially-trained cardiovascular physician and a cardiovascular team of nurses and technicians.
How long does the procedure last?
The cardiac catheterization procedure itself generally takes 30 minutes, but the preparation and recovery time add several hours to your appointment time. On your procedure day, it is best to plan on staying at Cardio of America all day for the procedure.
Angioplasty uses a balloon-tipped catheter to open a blocked blood vessel and improve blood flow. The doctor uses medical imaging to guide the catheter to the blockage. The balloon is inflated to open the vessel and improve blood flow. It may be done with or without a metal mesh tube called a stent. The stent is left inside the blood vessel to help keep it open. Angioplasty is minimally invasive and usually done under local anesthesia.
What is an atherectomy for atherosclerosis/PAD/PVD?
Atherectomy is a procedure that utilizes a catheter with a sharp instrument to remove plaque from a blood vessel. The catheter is inserted into the artery through a small puncture the artery. This is usually from the groin. The procedure is performed under local anesthesia. The catheter is designed to collect the removed plaque in which allows for the removal of the plaque as the device is removed from the artery. The process can be repeated at the time the treatment is performed to remove a significant amount of disease from the artery, thus eliminating a blockage from atherosclerotic disease. Why is this atherosclerosis atherectomy procedure performed? Why do I need this procedure? The goal of treatment is to eliminate the build-up of plaque in your arteries. You may need this atherectomy procedure if your arteries become too narrowed or blocked from plaque inside the artery walls. If arteries are blocked, blood cannot get through to nourish the tissues, causing the muscles of the lower extremities to cramp and lose strength.
How do I prepare for the atherectomy?
You may need to discontinue certain medications before the procedure. Your health care team will provide specific instructions to help you prepare. Other instructions are given on the day we schedule the procedure, and other instructions are provided.
What happens during the procedure?
The atherectomy will be performed under local anesthesia with a mild sedative given intravenously. Dr. Reddy will insert a catheter equipped with a shaving device and advance it through your artery until it reaches the area of blockage. Then passing it, the plaque is shaved away. The plaque will be collected and removed when the catheter is removed. Dr. Reddy may need to pass the catheter multiple times to remove a significant amount of atherosclerosis.
How long does the atherectomy procedure last?
The procedure itself may usually take 30-40 minutes, but the preparation and recovery time add several hours. Following the procedure, you will need to lie flat for at least 3 hours.
External Counter Pulsation
External Counterpulsation is a non-invasive, outpatient procedure designed to reduce the symptoms of angina pectoris (Chest Pain). The patient lies comfortably on a bed, and a series of blood pressure-type cuffs are wrapped around the legs. The cuffs inflate and deflate in sync with the heart to pump healthy blood throughout the body. Most patients read, listen to music, or even sleep during the treatments.
ECP consists of 35, one-hour-long treatments. Patients come in once a day, every day, for seven weeks
Expected Outcomes of Treatment
DO I NEED TO DO ANYTHING BEFORE HAVING ECP THERAPY?
Once you know you qualify for ECP therapy, there are a few helpful pre-treatment do’s, don’ts, and facts. First, you must understand that you are committing to one-hour sessions, five days per week, for seven weeks. Interruptions in the daily routine are not good and should be avoided if at all possible. You should plan to spend about an hour and a half each day at your treatment center. You may feel somewhat tired at the end of the first week, due to the “passive exercise” effect of ECP. Each day, your therapist will conduct a pre-treatment questionnaire, weigh you, and take your blood pressure before starting your therapy.
The following are recommend:
Exercise and Nuclear Stress Tests:
What is a Nuclear Scan?
A nuclear scan is a test that uses a radioactive substance, known as a tracer, to produce images of the heart muscle. When combined with an exercise test, the nuclear scan helps determine if areas of the heart are not receiving enough blood. NOTE: Nuclear tracer is not an iodine dye. The nuclear exercise scan is especially useful in diagnosing coronary heart disease that is the presence of blockages in the coronary arteries (the vessels that supply oxygen-rich blood to the heart muscle).
In most cases, doctors use two tracers during one test (dual-isotope imaging), one tracer for the rest portion (thallium), and the other for the exercise portion
What does it show?
During the test, a small amount of tracer is injected into a vein in your arm while you walk on a treadmill.
The tracer travels in the bloodstream is carried through the coronary arteries, and is picked up by the heart muscle cells.
Areas of the heart muscle that have an adequate blood supply pick up the tracer right away and more completely. Regions that do not have an adequate blood supply pick up the tracer very slowly or not at all.
The tracer gives off a small amount of radiation that is detected with a scanning camera. A computer processes the information and produces images of the radioactivity distributed in the heart.
If an area of the heart receives less blood than the rest of the heart (because of a blocked or narrowed artery), it will pick up less radioactivity and will show up as a lighter area, called a “defect.”
Preparing for the Test:
Do not eat or drink (except water) for 4 hours before the test. This will help prevent the possibility of nausea, which may accompany vigorous exercise after eating. Drinking plenty of water is okay.
If you are currently taking any heart medications, check with your doctor. He or she may ask you to stop certain medications a day or two before the test. If you are using inhalers for asthma or emphysema, please bring them with you. If you have any questions regarding your medications please call our office.
Before the test.
Once Scheduled you’ll be explained the procedure, and you’ll be asked to sign a consent form. Feel free to ask any questions before signing the consent.
Wear loose and comfortable clothing that is suitable for exercise, preferably a shirt or blouse that opens in the front. Also wear comfortable flat walking shoes or sneakers, no sandals or flip flops.
Several electrodes (small sticky patches) will be placed on your chest to obtain an electrocardiogram (ECG or EKG), a recording of your heart’s electrical activity. An intravenous (IV) line will be inserted into a vein in your arm to allow for injection of the tracer during exercise.
What Happens During the Test?
The nuclear scan is performed in the office at the hospital or at a test center. For one-day nuclear tests (most common), the rest portion is done first, then the exercise portion. In the two-day nuclear test, the rest portion is done one day, and the exercise portion is done another day.
Rest Portion
The tracer will be injected, and a set of pictures will be taken while you are at rest. You will lie flat on a unique table under a large scanning camera. During imaging, the camera takes pictures of your heart from various angles. Remain still while the pictures are being taken. This part of the test may take twenty (20) minutes. These images are compared to the images obtained during the exercise portion of the test.
Exercise Portion
You will walk on a treadmill. The treadmill moves slowly at first, then the speed and incline increase gradually.
If walking on the treadmill is not possible, you will receive an injection of a vasodilator to induce a chemical exercise. During infusion, you may experience chest pain, shortness of breath, headache, nausea, etc. These symptoms are transient and can be reversed within two (2) minutes with either cessation of the injection or another medication.
Be sure to report any symptoms, such as chest pain or discomfort, dizziness, or severe shortness of breath. Try to exercise for as long as you can, because it increases the accuracy of the test.
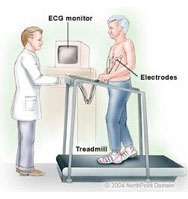
When you reach the point where you feel you can’t exercise for much longer, let the technician know. The technician will inject the tracer into the intravenous line. You will then be asked to continue exercising for another minute or so after the injection.
Another set of pictures will be taken. These images will be compared to the images obtained during the rest portion of the test.
How Long Does The Test Take?
For this test, allow four to five (4-5) hours for the entire examination, which includes preparation, the exercise portion, imaging waiting time.
Is This Test Safe?
The radiation exposure during a nuclear scan is small, and the doses used are safe. However, if you are pregnant, suspect you may be, or are a nursing mother, be sure to let the doctor and nuclear technician know. The exercise test is also safe. A small amount of risk does exist, however, because it stresses the heart. Possible complications include abnormal heart rhythms and chest pain. Experienced personnel is available to handle any emergency.
Your Test Results
Your doctor will discuss the test results with you during a future office visit. The test results help the doctor make an accurate diagnosis and develop a treatment plan that’s best for you.
ATTENTION: This is the preparation for the nuclear stress test.
Please read these instructions carefully:
You must fast (nothing to eat or drink except water) for four (4) hours before the test on the 1-day trial. You are encouraged to drink as much water as you can.
CAFFEINE and NICOTINE are NOT allowed for twelve (12) hours before the test.
Wear comfortable clothing, such as loose-fitting pants, T-shirts, etc. Your shirt must have NO METAL BUTTONS. Metal buttons interfere with the images and may result in an inaccurate test. Also, wear tennis shoes or sneakers. DO NOT WEAR BOOTS, HIGH HEELED SHOES, SANDALS, or FLIP FLOPS.
An echocardiogram is an ultrasound of the heart. A gel is applied to the chest, and the echo transducer is placed on top of it. The machine captures many pictures of the heart.
Is an imaging procedure that uses high-frequency sound waves ( Ultrasound) to view the carotid arteries. Viewing them allows us to determine if there is narrowing. This is the least invasive method utilized to evaluate for the presence of carotid artery disease.
A carotid duplex scan takes about 15 to 30 minutes and takes place in an ultrasound lab. The following steps take place during this procedure:
Ultrasound is a risk-free method to view changes and abnormalities in your body, including during pregnancy.
Peripheral artery disease (PAD) is usually diagnosed based on patients’ symptoms and physical examination in the clinic, confirmed by ultrasound evaluations in the Vascular Laboratory with pressure measurements and other non-invasive tests.
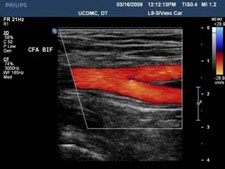
Ultrasound duplex scanning can provide additional information that may guide therapeutic decisions. The location and severity of arterial narrowing and occlusions can be identified. The vascular technologist can map disease in lower-extremity segments with high accuracy — though duplex scanning is more time-consuming than other lower-extremity arterial studies.
The additional information from duplex scanning can help determine if the arterial disease might be appropriately treated with endovascular intervention. The type of treatment and the technical approach can be guided by the duplex scan findings. Information from the duplex scan can help patients be better informed about their options. Duplex scanning after intervention can provide objective information about the success of the procedure, and serial follow-up examinations can identify recurrent problems at an early stage, sometimes prompting follow-up interventions.
Some preparation is needed. A complete lower extremity arterial evaluation includes duplex scanning of the aorta and iliac arteries in the abdomen and pelvis. Gas in the intestinal tract can interfere with ultrasound evaluation. It is, therefore, best to have the examination performed after an overnight fast and it is essential to avoid tobacco and caffeine before the test. A complete study can take up to 30 minutes.
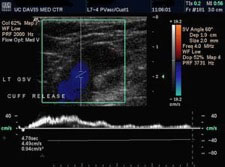
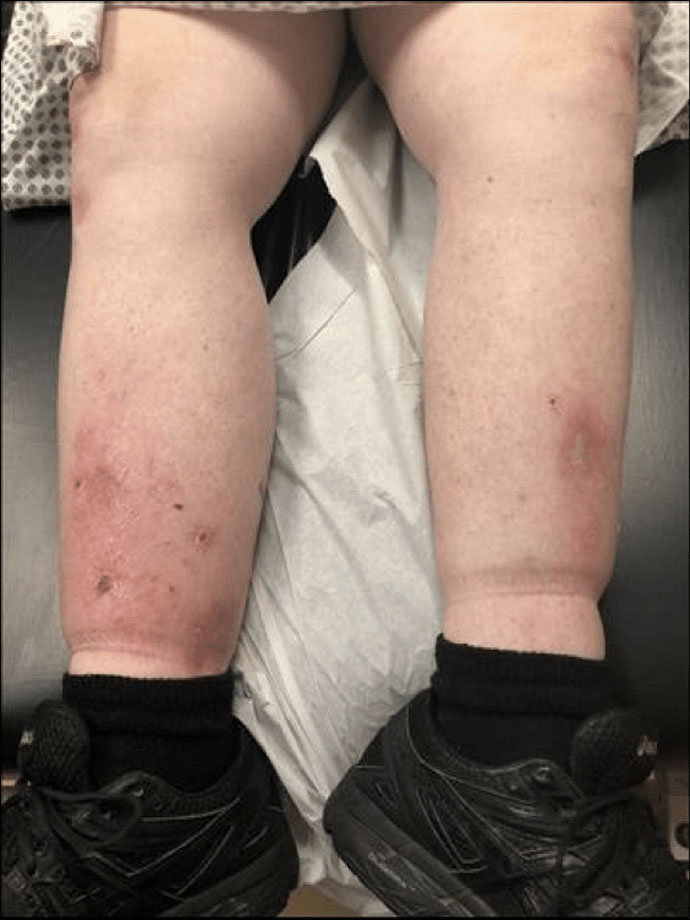
In the lower extremities, blood returns to the heart through a network of deep and superficial veins. Standard venous flow patterns depend on open venous channels and the function of numerous valves within the veins. Venous insufficiency may occur if veins are obstructed from a chronic thrombus (blood clot), for example, or if the valves are incompetent — no longer providing for only one-way flow. Venous valvular incompetence in superficial veins or communicating veins (veins that connect the deep and superficial veins) can result in varicose veins. Untreated chronic venous insufficiency in the deep or superficial venous system can cause progressive symptoms that include: pain, swelling, skin changes, and eventual tissue breakdown ( Ulcers).
Ultrasound scanning of the deep and superficial veins can be utilized to detect obstruction. Ultrasound also is used to evaluate the function of valves in each segment of the evaluated veins. Using Ultrasound(duplex scanning) the direction of blood flow can be evaluated. The examination is often done in the upright position, as this is the best way to evaluate valve function.
Evaluation of the function of the lower extremity veins is not needed in every case, but when surgical treatment, sclerotherapy, or saphenous venous ablation (closure) is being considered, a complete lower-extremity venous duplex scan can provide valuable information that may guide therapy. A comprehensive study may include both lower extremities.
No special preparation is required. A complete study usually takes about 30 to 60 minutes.
Treatment of venous insufficiency always includes the three “E’s” elevation of the leg, exercise, and use of elastic compression. In cases where intervention or surgery is considered, the duplex scan can provide essential information about which vein segments are abnormal, whether obstruction or reflux is present (or both), and how extensive a problem exists. This information will guide the vascular specialist’s recommendations and provide information that may help predict how successful treatment might be.
Pacemaker checks
Holter monitor
Implantable cardioverter-defibrillator (ICD)
check
What is Arrhythmias?
Arrhythmias are disorders that interrupt the regular rhythmic beating of the heart. They are relatively common. As many as 2 million Americans are living with Atrial fibrillation (one of many types of rhythm problems). Arrhythmias can occur in a healthy heart and be of minimal consequence or they may indicate a serious problem and lead to heart disease, stroke, or sudden cardiac death.
Holter Monitors
A Holter monitor is a portable device for continuously monitoring various electrical activities, may be either for 24 or 48 hours. Its extended recording period is sometimes useful for observing occasional cardiac arrhythmias that would be difficult to identify in a shorter period or on a single Electrocardiogram( EKG/ECG). For patients having more transient symptoms, a cardiac event monitor can be worn for a month.

What is a natural pacemaker?
The heart’s “natural” pacemaker is called the sinoatrial (SA) node or sinus node. It’s a small mass of specialized cells in the top of the right atrium or chamber of the heart. It makes the electrical impulses that cause your heart to beat.
A chamber of the heart contracts when an electrical impulse moves across it. For the heart to beat correctly, the signal must travel down a specific path to reach the ventricles, the heart’s lower chambers.
The natural pacemaker may be defective, causing the heartbeat to be too fast, too slow, or irregular. The heart’s electrical pathways also may be blocked.
What is an artificial pacemaker?
An “artificial pacemaker” is a small, battery-operated device that helps the heartbeat in a regular rhythm. Some are permanent (internal), and some are temporary (external). They can replace a defective natural pacemaker or blocked pathway.
A pacemaker uses batteries to send electrical impulses to the heart to help it pump properly. An electrode is placed next to the heart wall, and small electrical charges travel through the wire to the heart. Most pacemakers have a sensing device that turns itself off when the heartbeat is above a certain level. It turns back on when the pulse is too slow. These are called demand pacemakers.